Treatment of patients with relapsed or refractory myeloma
Efstathios Kastritis, MD
National and Kapodistrian University of Athens
Several presentations provided updated data and new information of new combinations for the treatment of patients with relapsed of refractory myeloma. 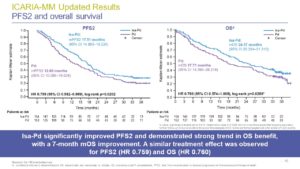
The ICARIA study compared isatuximab plus pomalidomide with dexamethasone vs pomalidomide with dexamethasone in patients with relapsed/refractory myeloma and at least 2 lines of therapy,. Dr A. Perrot presented the updated follow up (Abstract S186) after ~35 months of median follow up, showing that Isa-Pd was associated with significant benefit in PFS (11.1 vs 5.8, HR 0.599), time to next treatment (15.5 vs 8.9 months, HR: 0.555), in PFS2 (17.5 vs 12., HR 0.759) and in OS (24.6 vs 17.7, HR 0.760). Subsequent therapy with daratumumab in those that received Isa-Pd was associated with shorter PFS than in those that received Pd. Response rates in patients that received daratumumab monotherapy were lower in those that had received Isa-Pd than in those that received Pd (14.3% vs 37.9%) but when combinations of daratumumab with other agents were used response rates were similar (30.8% vs 31.8%)
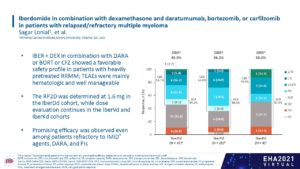 Prof. S. Lonial presented the data from a phase 1 study with multiple cohorts that evaluated several regimens with iberdomide including combinations with daratumumab (n=43), bortezomib (n=25) or carfilzomib (n=9) (Abstract S187). About one third of patients were triple-class refractory. Non-hematologic toxicity was low and the dose of Iberdomide for combination with daratumumab was 1.6 mg, while dose evaluation continues for Iber-Vd and Iber-Kd. The best ORR was 45.9% with Iber-DaraD (mostly in Daratumumab-naïve patients), 56% with Iber-Vd and 50% in Iber-Kd.
Prof. S. Lonial presented the data from a phase 1 study with multiple cohorts that evaluated several regimens with iberdomide including combinations with daratumumab (n=43), bortezomib (n=25) or carfilzomib (n=9) (Abstract S187). About one third of patients were triple-class refractory. Non-hematologic toxicity was low and the dose of Iberdomide for combination with daratumumab was 1.6 mg, while dose evaluation continues for Iber-Vd and Iber-Kd. The best ORR was 45.9% with Iber-DaraD (mostly in Daratumumab-naïve patients), 56% with Iber-Vd and 50% in Iber-Kd.
Prof. Gasparetto presented at EHA (Abstract S188) the results of a study that evaluated once weekly oral selinexor in combination with Kd (with carfilzomib also given once weekly) in patients with relapsed or refractory MM (median 4 prior lines but carfilzomib non-refractory). The recommended phase 2 dose was selinexor 80 mg weekly and carfilzomib 56 mg/m2 weekly. Thrombocytopenia was the most common hematologic toxicity while GI toxicity was common but rarely was grade 3. The ORR among the 32 patients was 78% (sCR/CR: 15.6%, VGPR: 25%), similar also in patients with high-risk cytogenetics and the median PFS was 15 months; in the subset of pates with triple-class refractory disease median PFS was 23.7 months.
The BOSTON study compared selinexor plus Vd (XVd) vs Vd in patients with RRMM and 1-3 prior lines of therapy. Prof. T. Facon presented at ASCO (abstract 8019) a post-hoc survival analysis for patients of different age groups was compared (≥65 vs < 65 years). Median PFS was prolonged with XVd vs Vd, across both age groups (in ≥65 HR was 0.55 and in < 65 HR was 0. 74). The median OS was not reached in patients ≥65 with XVd vs 28.6 months with Vd (HR = 0.60). There was no increased toxicity with XVd in those ≥65 and polyneuropathy rates were lower with XVd vs Vd.
Why Become a Member
The International Myeloma Society is a professional, scientific, and medical society established to bring together clinical and experimental scientists involved in the study of myeloma. The purpose of this society is to promote research, education, clinical studies (including diagnosis and treatment), workshops, conferences, and symposia on all aspects of multiple myeloma worldwide.
The IMS is a membership organization comprised of basic research scientists, and clinical investigators in the field along with physicians and other healthcare practitioners.

